Bunion
What is a bunion?
Bunions are primarily a hereditary condition and most often progressively worsen throughout life. They can affect anyone, although they are most common in women. Bunions will usually be visibly present for many years before they become painful. A change of shoes, activity, or body weight can cause previously non-painful bunions to become painful. A bunion occurs due to multiple factors which result in a mal-alignment of the bones with the big toe drifting toward the second toe. Additionally, there is an enlargement of the “bump” on the inner side of the foot, next to the big toe. As a bunion deformity progresses, the “bump” or bony enlargement increases in size. In addition, the big toe can rotate, and continues to move towards, often over-lapping or under-lapping the second toe.
A bunion is a bone problem. It is not a skin problem or a cyst. As you walk more the symptoms become worse. As the bunion increases in severity it can cause other associated foot problems, such as hammertoes, arch pain, and painful calluses on the bottom of the foot.
Pain is often the result of rubbing of the enlarged bunion against the inner side of a shoe. There may be pain from within the actual bunion joint or when the great toe presses against the second toe.
The exact cause of bunions is unclear. Some of the causative factors include heredity, flat foot structure, ligamentous instability or laxity, muscular imbalance within the foot and birth defects. Improper shoes during childhood may contribute to the formation of bunions, but this is uncommon. Inappropriate shoes during adolescence and early adulthood may aggravate an existing bunion formation.

Mild Bunion

Moderate Bunion

Severe Bunion
Can lasers eliminate bunions?
This much-publicized technique is misleading. It is impossible for a laser to cut bone or correct a bunion. Making precise bone cuts is the most critical and important part of a successful bunionectomy. Lasers are useful for very few foot procedures, and offer minimal benefits over traditional techniques.
What’s unique about our approach to bunion correction?
In order to effectively correct a bunion and reduce recurrence, all of the foot changes must be addressed to ensure appropriate function after the surgery. Simply removing the visible “bump of bone” will rarely produce a long-lasting result, and does not address the internal structural problems. Unfortunately, inappropriate bunionectomies address only the “bump of bone.”

Surgical Screw
(gold plated titanium alloy)
Our technique includes realigning the bone for proper function, and uses a surgical screw for the most reliable and stable bone alignment. The proper use of the surgical screw is technically more difficult than other methods, but is worth the additional time and effort. There are several other methods of fixation that can be used in performing a bunionectomy. The screw provides the greatest amount of compression, strength and stability. (Just like screws rather than nails are used in manufacturing excellent furniture, similar thinking is used in our bone fixation.)
Some patients request the removal of the screw after the surgery. If required, the screw can be removed easily during a ten minute office procedure. This procedure may be performed three months after the surgery.
The screw will not affect the security metal detectors at airports.
This method decreases pain, shortens the recovery time, allows for a more rapid return to regular activities and decreases the chances for a recurrence.
See time line for bunionectomy to determine recovery time.
Do bunions ever return?
No surgeon can guarantee perfect results. Unfortunately, if the wrong procedure is performed, the recurrence rate can be quite high. Many of the micro-surgeries and laser techniques have a high recurrence rate because they generally cannot accurately realign the bones. These types of procedures have become less popular recently due to the incidence of recurrence as well as other problems.
There are several bunion procedures. The choice of the correct bunion procedure is critical. The skill of the precision in which the bone is cut, shaped and realigned is essential in producing an excellent result.
When should I have my bunions corrected?
If you have any of the following problems, your feet should be evaluated:
- Calluses on the inside of the big toe
- Pain around the big toe when wearing certain shoes
- Painful calluses on the bottom of your feet
- The big toe pushing on the second toe
- Difficulty wearing shoes or participating in activities, sports or dancing
- Increasing need to wear wider shoes
Results of the Angulated (Tri-plane) Bunionectomy:
In the past, bunion sufferers have been subjected to an array of surgical procedures with mixed results. Pain, long-term disability, hospitalization and casting were the standards of care. Now we use a procedure which changes the traditional way in which bunions are approached. This bio-engineering technique realigns the bones and maintains the correction securely and with generally minimal discomfort. Our results have been very impressive.

Pre-operative X-ray
Traditional Bunionectomy
- Often done under general anesthesia and may require inpatient hospitalization.
- Many times require a cast or painful steel pins which protrude through the skin.
- Often minimal walking with crutches for months after the surgery.
- Patients cannot wear shoes for prolonged periods of time. Extensive pain medication is often required.

Post-operative X-ray with screw
Angulated Bunionectomy
- Performed under a local anesthesia, or with mild sedation (twilight sleep) on an out-patient basis (no overnight stay).
- A surgical screw is placed beneath the skin. Nothing protrudes through the skin. There are no casts, crutches, or walkers after the surgery. Only a soft gauze dressing is used.
- Most patients walk immediately after surgery without crutches, using only a surgical shoe or sandal.
- Patients usually return to tennis shoes after two weeks, with minimal discomfort. Minimal pain medication usage is common.
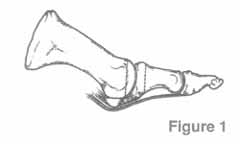
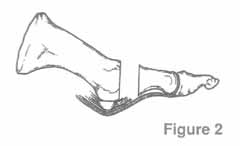
This is the surgical shoe that is worn for two weeks after the surgery.

Surgical Shoe
Casting is not required. Crutches, canes or walkers are rarely used.
What happens if I have arthritis in my joint?

Bunion X-ray
The nature of a bunion is not just a bump. As the “bump” increases in size, often the great toe pushes laterally toward the second toe. This is generally the moderate stage of the development of a bunion. As the joint continues to function out of alignment, the bunion deformity gets worse. Some bunion deformities worsen more rapidly than others, but they all get worse with time.
In more advanced stages, some patients also develop osteoarthritis (wearing down of the bunion joint.) The longer the joint is crooked and the longer the joint is mal-aligned, the greater the chance for the person to develop arthritis.
This x-ray on the left shows a foot with severe arthritis of the bunion joint (1st MPJ or metatarsophalangeal joint), and less arthritis of the smaller toe joints. Notice how enlarged the bunion joint has become due to the extra bone growth around the joint.
Traditionally, arthritic joints were destroyed or fused.These are not good alternatives for an active person who puts great demand on their feet. Why destroy a joint if you can save it? For many patients with severe arthritic bunions, a bunionectomy with joint replacement can be used. An MP joint replacement is similar to a hip joint replacement. The results are generally excellent for reducing joint pain and allowing increased activity.Using surgical engineering, we are able to get the big toe joint to bend again, saving many such arthritic joints.
Excellence in surgical engineering
The foot is an amazing mechanical apparatus. What’s surprising is how important the bunion joint really is. If the bunion joint doesn’t function correctly, many people not only have foot pain, but often unconsciously walk awkwardly to avoid putting additional stress on the painful area of their foot. This is why so many people with big toe problems also develop knee and back pain.
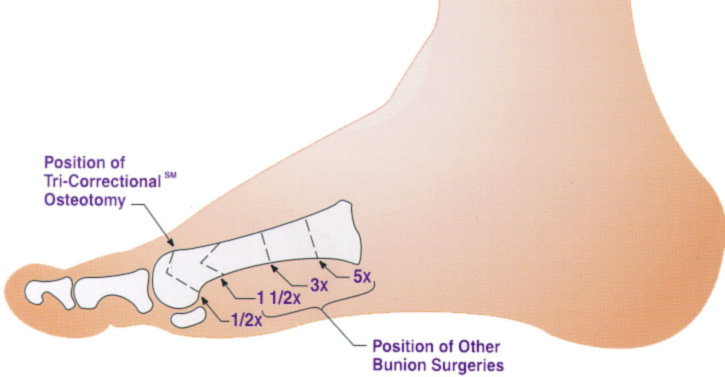
Placement of the Angulated Osteotomy
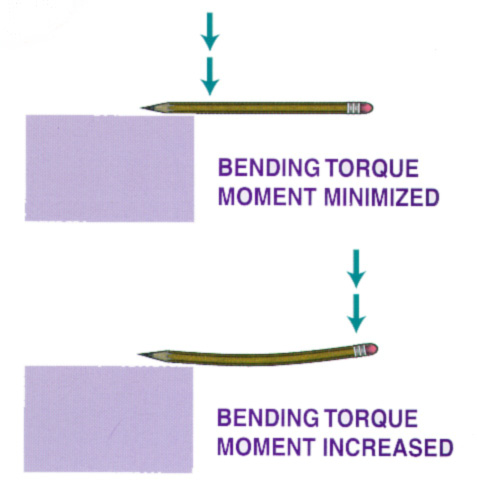
Pencil Example of Bending Torque Moment
Since the force on the big toe joint is horizontal, bending torque moment occurs when you walk. Bending torque moment measures the point of application of weight-bearing forces times the length of the metatarsal bone (lever arm) to the osteotomy location (bone cut). The application of Angulated Bunionectomy (at 1/2x) minimizes the bending torque moment. The illustration below shows the placement of the angulated osteotomy as compared to other traditional osteotomies:
As the osteotomies are moved farther away from the big toe joint, the bending torque moment becomes higher. Higher bending torque moment creates more stress in the area of the bone cut, which can prolong recovery time. Other bone surgeries are done similarly, but there is an advantage in performing surgery at the end of the bone to minimize torque. The quality of the bone is better closer to the joint. The better the quality of bone, the faster the bone heals. Our goal in creating the Angulated Bunionectomy was to minimize torque so that we can get you back to your activities as quickly as possible.
The effects of bending torque moment are similar to bending of a pencil whose point is placed on the edge of a table. Applying a force near the tip of the pencil will not generally result in breaking the pencil, because bending torque moment is minimized. But, if one applies the same force near the eraser, the pencil will break much more readily.
What is my foot going to look like after surgery?
While the Angulated Bunionectomy is performed to repair your painful joint, it is also used to repair unsightly feet. Many people with bunions are embarrassed by their appearance. The Angulated procedure has helped many people return to a life of open-toed shoes.


Before

After
Most of our patients experience minimal discomfort
This new bioengineering procedure, the Angulated Bunionectomy, is done on an outpatient basis. Historically, bunionectomies were performed in the hospital where patients stayed overnight, usually due to post-operative pain and their inability to walk.
Most of our patients stated that their discomfort was markedly less than they had anticipated, and required minimal medications for pain. Additionally, the surgical engineering approach stabilizes the bone allowing our patients to walk the same day as their surgery.
The majority of our patients are in shoes after two to three weeks
With traditional bunion surgery, a return to shoes has often been delayed by pain, swelling, and the inability to walk because of pins or bone instability. The use of a surgical screw significantly reduces pain and swelling. Security of the bone realignment usually allows for immediate weight bearing and ambulation without the need for any casting. Patients are generally ready to begin wearing shoes two weeks after surgery. (See Time Line for Bunion Surgery).
In the past, pins and wires were used to hold the alignment of the bones. The pins stuck out of the foot and prolonged the return to shoes by as much as a month or more. The surgical screw we use is placed beneath the skin and is far more stable than pins. To ensure the best possible results, patients often enter a program of vigorous rehabilitation to help with the healing process and increase the flexibility of the corrected joint.
Bunion with Stiff and Painful Toe Joint
With a more advanced bunion, there is often pain and a decrease of motion of the first metatarsophalangeal joint (1st MPJ) or bunion joint. This type of pain is generally felt within the joint rather than on the surface. Normally the range of motion of the 1st MPJ is about 60 degrees. With an advanced bunion, (often called a hallux limitus), there can be as little as no motion in the joint. Frequently there is significant arthritis associated with the 1st MP joint, which is clearly visible on x-ray. In addition to the arthritis, there may be dislocation of the 1st MPJ.
There are several causes of hallux limitus. Due to age, there may be a gradual deterioration of the joint. There could be a history of trauma to the foot or joint. Old sports injuries could have initiated this type of problem.
Different grades of the deformity exist from mild to severe, with the amount of joint motion typically decreasing over time. Patients usually exhibit pronated or flat feet during gait and stance.
Orthotics are an important conservative therapy because they can help control the abnormal pronatory forces that are created during walking. Orthotics can serve as an alternative treatment to surgery during the early stages. They also can act as a postoperative tool to limit the biomechanical influences that caused hallux limitus, thus reducing the chance of reoccurrence of symptoms.
Surgical Options
When the conservative option of using orthotics is ineffective, then surgery should be considered. The surgical procedure consists of a specialized bunionectomy procedure, where the abnormal and arthritic portion of bone of the bunion joint is removed and it is replaced by an implant or joint replacement (see picture). The procedure is referred to as a Bunionectomy with an Joint Replacement. If the bunion deformity is not as severe, or if there is little stiffness or joint pain, then the Angulated Bunionectomy is generally the better choice. The Bunionectomy with Joint Replacement procedure takes approximately 40 minutes, and can be performed as an outpatient. Patients can walk on the foot, using a special surgical shoe, immediately after the surgery, without crutches, walkers or a cast. Time Line for Bunion Surgery will provide additional details. If you wish to see the actual intra-operative photographs of this procedure, please request the URL by sending us an e-mail.
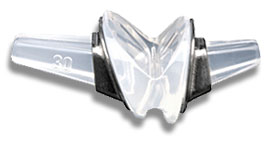
Futura Joint Replacement
This is a photograph of the Futura joint replacement. It is available in a variety of sizes, depending upon the size of the foot. The upper and lower “stems” of the implant fit inside the metatarsal and great toe bones. The hinge part of the implant is positioned between the metatarsal and toe bones.
A side view of the bunion joint area before the procedure.
Notice the two vertical lines drawn on both sides of the joint.
The section of the worn or degenerated joint has been removed.

View from the top of the foot with the Futura Primus joint replacement positioned in the joint space. No screws or cement is used in this procedure.

Side view of Figure 4. Notice the angled positions of the stems within the bones. These angled stems improve the function of the joint.

This pre-operative x-ray of a left foot shows the severe bunion “B” and the great toe “T” pushing against and causing a hammertoe “HT” of the adjacent 2nd toe. Note the dislocation “D” of the joint, as it is almost “falling off” the side of the bone.

This post-operative x-ray of the above left foot, shows the results of the surgery. The implant or joint replacement “I” is positioned at the old location of the dislocation. The bunion “B” is removed, and the great toe “T” is now straight. In addition, the 2nd hammertoe “HT” is corrected and straight.
This is the surgical shoe that is worn for two weeks after the surgery. Casting is not required. Crutches, canes or walkers are rarely used.

Surgical Shoe
Tailor’s Bunion
What is a Tailor’s Bunion?
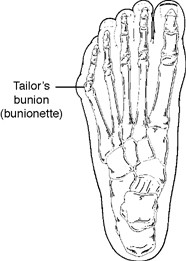
Bunionette
Tailor’s bunion, also called a bunionette, is an enlargement of the head of the fifth metatarsal bone near the base of the little toe. Tailor’s bunions are not as common as bunions, which occurs at the big toe, but both are similar in symptoms and causes.
The symptoms of tailor’s bunions include redness, swelling, and pain at the site of the enlargement. These symptoms occur when wearing shoes that rub against the enlargement, irritating the soft tissues underneath the skin and producing inflammation.
Why do we call it “tailor’s bunion”?

The fifth metatarsal bone starts to protrude outward.
The deformity received its name centuries ago, when tailors sat cross-legged all day with the outside edge of their feet rubbing on the ground. This constant rubbing led to a painful bump at the base of the little toe.
Causes of a Tailor’s Bunion
A tailor’s bunion is caused by an inherited change of the mechanical structure of the foot. The fifth metatarsal bone starts to protrude outward, while the little toe moves inward. This shift creates a bump on the outside of the foot that becomes irritated whenever a shoe presses against it.
Conservative Treatment
Shoe modifications. Choose wide shoes, and avoid those with pointed toes or high heels.
Oral medications. Non-steroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen, may help relieve the pain and inflammation.
Padding. Pads placed around the area may help reduce pain.
Icing. An ice pack may be applied to reduce pain and inflammation.
When is Surgery Needed?
Surgery is often considered when pain continues despite the above approaches. Surgery is highly successful in the treatment of tailor’s bunions. If the above is not effective, then the excessive bone spur needs to be surgically shaved or remodeled.